Fall 2021 Newsletter

By Rebekah Csonka, OTS
Occupational Therapy, University of Central Arkansas
Faculty Mentor: Lorrie A. George-Paschal, Ph.D., OTR/L, ATP
Expert Mentor: Kerry Jordan, PhD, RN, CNS, CNL-BC
Site Supervisor: Mrs. Kim White
Site Contact: Mrs. Debra Robinson
The life changes that older adults experience as they age such as loss of a spouse, and changes in housing, health status, and income, can cause many older adults to be at an increased risk for loneliness. Research shows that loneliness is a risk factor for mortality and is comparable with other behaviors that promote negative health outcomes such as obesity and substance abuse, therefore, it is imperative that loneliness be addressed among the older adult population (Holt-Lunstad et al., 2015). Research shows that engagement in leisure, social, physical, and community activities have a positive impact on older adults’ overall health (Stav et al., 2012). Therefore, occupational therapists, due to their unique ability to promote engagement socially through meaningful activities, can play an integral role in the lives of older adults experiencing loneliness by providing interventions targeting social engagement.

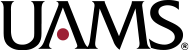
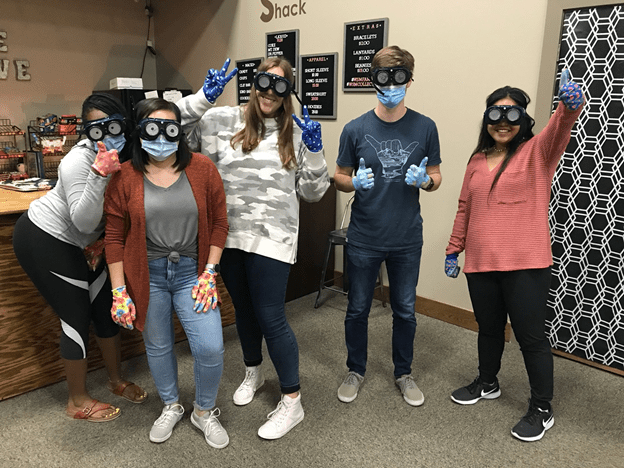
To address feelings of loneliness and decreased community and social engagement among older adults, UCA occupational therapy student, Rebekah Csonka along with the guidance and support of her expert mentors from UCA’s occupational therapy and nursing department, developed a community program as part of her student doctoral capstone project called “Sparking Community Engagement Through Occupations: Individual Guidance and Peer Support for Older Adults Experiencing Loneliness.” This community program is composed of two parts. The first half of the program focuses on meeting with each older adult weekly, collaborating with them to create goals for social and activity engagement, and carrying out their goals in the community. For the second half of the program, the older adults participate in a small peer social group, at the Maumelle Center on the Lake and the Faulkner County Senior Wellness and Activity Center, where activities chosen for social and community engagement promote relational building and engagement among group members as well as community participation. This program currently has six older adults participating who have self-reported feelings of loneliness or whose families have identified a need for increased social or activity engagement.

By the end of the first half of the program, these older adults show an increase in their social and community engagement and have found support through relationships built with other older adults in the community. One lady in the program, Mrs. M, had a goal to volunteer in the community. Together, we identified her strengths and previous experiences to find that she would be a wonderful support to families going through the process of losing a loved one. She is pictured holding paper flowers, as one of her sessions was spent identifying activities that she can do for or with people that she will be serving in the community, as a hospice care volunteer. Another community-dwelling older adult, Mrs. C, had a goal to make social connections with others. She is pictured standing outside of the Faulkner County Extension Office after attending her first class through the Extension Get Fit Program, where she had the chance to make connections with other older adults while engaging in an exercise program. She looks forward to staying engaged in this group to make new friends and to feel a greater sense of support and social connections. Hopefully this capstone project will pave the way for future community programs that will focus on the needs of older adults for social and community engagement through meaningful occupations.
References
Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., & Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science, 10(2). 227-237. https://doi.org/10.1177/1745691614568352.
Stav, W. B., Hallenen, T., Lane, J., & Arbesman M. (2012). Systematic review of occupational engagement and health outcomes among community-dwelling older adults. American Journal of Occupational Therapy, 66(3). 301–310. https://doi.org/10.5014/ajot.2012.003707