Fall 2021 Newsletter

By Robin McAtee, PhD, RN, FACHE, Director, Arkansas Geriatric Education Collaborative (AGEC), a Geriatric Workforce Enhancement Program (GWEP) at the University of Arkansas for Medical Sciences (UAMS) Donald W. Reynolds Institute on Aging (DWR IOA)
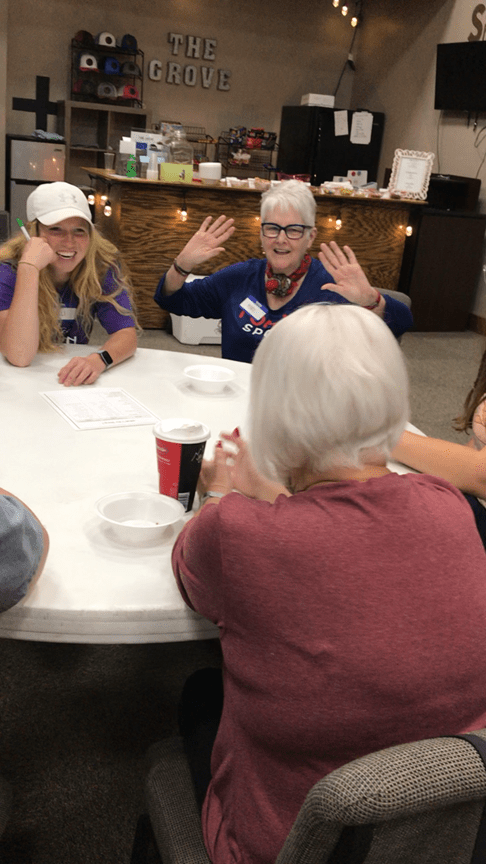
Hello from the Arkansas Geriatric Education Collaborative. As summer of 2021 ends and we begin to enjoy the cooler nights and days, we are beginning one of the busiest times of the year here at the AGEC. I know by this time we had all hoped that we would be on the “other side” of the pandemic, but we still seem to be simmering in the middle and we are all getting weary! However, despite the weariness, we have adapted and thrived in many areas. Our summer was full of exciting programs and we are still developing new partnerships, programs, and activities as we explore new methods and platforms for reaching older adults and healthcare professionals with geriatric content. Our healthcare professional webinars continue to be huge successes. In September, we had Dr. Anand Venkata who talked about COVID-19 Long Haulers: Pulmonary Complications – What to Expect, and we had 161 attendees. On October 7, Dr. Lee Isaac with UAMS PRI presented Diversity in Dementia: Incidence, Related Factors, and Considerations for Diagnosis and Treatment with 131 attendees. Our social media presences (Facebook, Twitter, and Instagram) are still growing with a lot of views and activities, so be sure to check those out. We are also having a few, socially distant, face to face, evidence-based programs and older adults seem to enjoy getting out again! In addition, many of our community-based partners are once again providing both in-person and virtual programs and activities. Many of the senior centers are open again and providing programs and UAMS Centers on Aging also reported that they are once again out in the communities they serve, providing caregiver workshops and training first responders.
Our academic partners were busy during the summer. Our team had an intern from Hendrix who worked with AGEC outreach and social media activities. UCA opened a new interprofessional clinic where education and resources are provided for caregivers. ASU graduate nursing students began working on quality improvement projects at local long-term care facilities. Each college reported that activities are picking up more this fall with students being on-campus more and are actively engaging in geriatric clinical activities.
We continue to seek new ways to reach and teach all audiences and if you have any suggestions, please let us know. Happy Fall!!!

Robin E. McAtee, PhD, RN, FACHE